Vitamin D deficiency linked with decreased pregnancy rates in IVF
1. In women undergoing IVF, vitamin D deficiency was associated with a lower clinical pregnancy rate compared with an adequate serum vitamin D level (≥20ng/mL).
2. Vitamin deficient women also experienced significantly lower rates of embryo implantation than those who had sufficient vitamin D levels.
Evidence Rating Level: 2 (Good)
Study Rundown: Over 30 years of research in animal models demonstrate a role for vitamin D in reproductive function whereby a diet low in vitamin D is associated with severely impaired fertility. Mice deficient in 1α-hydroxylase, the enzyme that catalyzes conversion of the storage form of vitamin D (25-hydroxy vitamin D) to the biologically active form (1,23-dihydroxy vitamin D) are infertile, with uterine hypoplasia and absent corpora luteae. Existing data suggests vitamin D might play a role in fertility on one ore more levels by permitting cyclical oocyte development, embryo implantation, and/or physiologic hormone regulation across the hypothalamus-pituitary axis. It is known that most human reproductive organs contain vitamin D receptors but few studies have replicated results in humans. Of the existing studies, results are mixed and designs have been limited by small sample sizes and homogenous populations.
In the present work, the largest human study to date, researchers evaluated the association between vitamin D deficiency and clinical pregnancy rates among women undergoing IVF. Results demonstrated that vitamin D deficient women are less likely to become pregnant and also experience lower rates of embryo implantation. Strengths include prospective design and assessment of a priori confounders, including BMI. Limitations include assessment of the storage form of vitamin D, not the biologically active form. The study population was >90% Caucasian Italian women, thus the results may not be generalizable to other populations, including populations of women with a higher incidence of fibroids and of course women without infertility. An allowable time window of 90 days between Vitamin D measurement and embryo transfer may alter results such that the impact of Vitamin D when it matters most, at the time of embryo transfer, was not assessed.
A randomized controlled trial with four arms (Group 1: adequate Vitamin D, Group 2: deficient Vitamin D; randomized to vitamin D vs. placebo) characterizing the association of Vitamin D serum measurement on the day of embryo transfer with live birth rate would inform clinical decision making in women undergoing IVF and potentially alter preconception counseling in the general population.
Click to read the study in JCEM
Relevant Reading: Relevance of vitamin D in reproduction
In-Depth [prospective cross-sectional study]: Reproductive age women with normal BMI and adequate ovarian reserve presenting to an university-affiliated Italian infertility center from January 2012 through December 2012 were eligible for inclusion. Serum vitamin D levels (25(OH)D) were measured at the beginning of IVF cycle preparation. The primary outcome was clinical pregnancy rate per embryo transfer, defined as a viable fetus on transvaginal ultrasound. A secondary outcome was implantation rate, calculated as the number of sonographically viable gestations divided by embryos transferred.
Of the 335 women recruited, 154 were vitamin D deficient (serum 25(OH)D<20ng/mL). Women with sufficient levels of vitamin D (≥20ng/mL) were more likely to become pregnant after IVF than those who were deficient (31% vs. 20%; OR:2.15, CI:1.23-3.77). Vitamin D sufficient women had higher rates of successful embryo implantation (OR=1.91, CI:1.20-3.05).
More from this author: Contained morcellation for benign gynecologic surgeries feasible, minimize surgical risk, Oocyte vitrification not associated with adverse obstetric or perinatal outcomes, IUD contraception equally safe in teenagers as in older women, No-cost contraception reduces unintended pregnancy rates, 20% lifetime risk of pelvic floor surgery in women
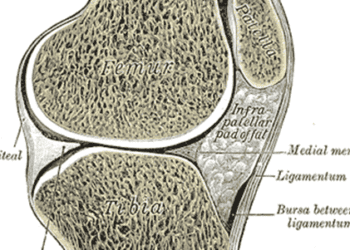
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.