Wellness Check: Sleep
Sugar-sweetened beverage intake may be associated with lower sleep duration in children
1. In this cross-sectional study, household food insecurity and daily servings of sugar-sweetened beverages were associated with sleeping less than the recommended sleep duration in children 4-60 months old who were supported by the Special Supplemental Nutrition Program for Women, Infants, and Children.
2. Furthermore, each additional serving of sugar-sweetened beverages was associated with increased odds of sleeping less than the daily recommended sleep duration.
Evidence Rating Level: 3 (Average)
Child development is dependent on several factors, including optimal sleep duration. Although prior studies have investigated the role of sleep duration on health outcomes in children, few studies have looked at this association in young children under the age of 5. Given that approximately one-third of children ages 4-60 months have insufficient sleep, this represents an opportunity for exploration. Furthermore, social determinants, such as food insecurity and socioeconomic status, may impact sleep quality in young children. Therefore, the present study aimed to investigate the household and social factors that may impact sleep duration in children under the age of 5.
This cross-sectional study included 9,547 children ages 4-60 months who lived in households supported by the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in Los Angeles County (LAC). Data from the 2017 and 2020 WIC LAC WIC survey was obtained from the child’s caregiver. Caregivers were included if they were 18 years or older, were receiving WIC for themselves or their child, and lived in LAC. The WIC survey included questions regarding the household environment, health insurance coverage, food intake, sleep duration, and more. Participants were asked how many hours the child slept in a typical day, and this was compared to the sleep recommendations set by the National Sleep Foundation (NSF) and the American Academy of Sleep Medicine (AASM). The primary outcome was the classification of participants into one of three groups based on their sleep duration relative to the sleep recommendations: sleeping less than the recommended sleep duration (LTR), being in the recommended range of sleep duration, or sleeping more than the recommended sleep duration (MTR).
The results demonstrated that food insecurity and daily servings of sugar-sweetened beverages were associated with LTR sleep in children 4-60 months old. Furthermore, there was a direct association between sugar-sweetened beverages and sleep, whereby each additional serving of these beverages resulted in an increased risk of LTR sleep. Other social factors also influenced sleep. Caregivers without practical or social support, or children of caregivers with a high school education or less were more likely to get LTR sleep. However, the study was limited by the caregiver’s reports of sleep duration, which may have introduced bias and inaccuracies in the reported sleep durations. Nonetheless, the present study demonstrated that several social factors may contribute to sleep duration in young children.
Sleep duration may be linked to periodontitis and tooth loss in adults
1. In this cross-sectional study, there was a significant association between insufficient sleep duration and the presence of moderate or severe periodontitis and tooth loss.
2. Furthermore, both insufficient and excessive sleep were associated with increasing periodontitis.
Evidence Rating Level: 3 (Average)
Periodontitis is a highly prevalent condition and is the main cause of tooth loss. Periodontitis and tooth loss can precipitate other problems, such as sleep disruption, low mood, and cognitive impairments. Sleep loss can be an outcome of periodontitis and tooth loss but can also be a precipitant of this condition. Sleep loss is known to activate inflammatory pathways, which can contribute to oral disease. Although several studies have identified a link between periodontitis and sleep loss, little research has been done to investigate the link between sleep duration and the development and progression of periodontitis. Therefore, the present study aimed to assess the association between sleep duration and periodontitis and investigate the factors affecting this relationship.
This cross-sectional study included 35,636 participants who completed the National Health and Nutrition Examination Surveys (NHANES) between 2005 and 2020. Participants were excluded from the analysis if they were under 30 years old, or if they had missing data regarding sleep duration, periodontal examinations, or relevant covariates. Data on sleep duration was determined from the NHANES and participants were classified into one of four groups: insufficient sleep (2-6 hours), adequate sleep (7-8 hours), excessive (9-12 hours), and continuous. Information on periodontitis was also obtained from the NHANES and participants were classified as having none, mild, moderate, or severe periodontitis based on the American Periodontal Association criteria. The primary outcomes were periodontitis and tooth loss.
The results demonstrated that there was a significant association between insufficient sleep duration and the presence of both moderate to severe periodontitis and tooth loss. There was a U-shaped pattern between sleep duration and periodontitis—periodontitis was most prevalent in those with inadequate or excessive sleep and lowest in those with adequate sleep. In looking at mediating factors, it was found that blood pressure explained approximately 7% of the relationship between sleep duration and tooth loss. However, the study was limited by the use of self-reported measures for sleep duration, which may have introduced bias. Nonetheless, the present study demonstrated that sleep duration is closely associated with periodontitis and tooth loss.
Freezing of gait is associated with sleep disorders in patients with Parkinson’s disease
1. In this systematic review, Parkinson’s disease patients with freezing of gait (FOG) experienced overall worse sleep quality, increased daytime sleepiness, and more disruptive sleep disturbances than those without FOG.
2. Furthermore, Parkinson’s disease patients with FOG had a higher likelihood and greater severity of rapid eye movement behavior disorder than Parkinson’s disease patients without FOG.
Evidence Rating Level: 1 (Excellent)
Patients with Parkinson’s disease (PD) experience several motor and cognitive effects. Sleep disorders are also highly prevalent in PD patients, which can have a significant impact on their quality of life. One motor symptom, freezing of gait (FOG), is suggested to be linked to sleeping disorders in these patients. Previous research has found that FOG and sleep share a bidirectional relationship, whereby those with FOG report more sleep disturbances, and those with sleep disturbances have an increased risk of developing FOG. However, no review has summarized the evidence regarding the association between FOG and sleep disorders in PD patients. Thus, the present study aimed to compare the sleep outcomes in PD patients with FOG (PD+FOG) and without FOG (PD-FOG).
Of 147 identified records, 20 studies were included in the review. Studies were included if they were conducted on PD patients aged 18 years or older and reported on any measurement of sleep and FOG in individuals. Studies were excluded if they were case reports, abstracts, editorials, case studies, or meta-analyses. The review was carried out in accordance with PRISMA guidelines. The study quality was evaluated using a customized quality checklist. The primary outcome was the prevalence of sleep disturbances and disorders in patients with PD+FOG and PD-FOG.
The results demonstrated that PD+FOG patients experienced more severe sleep disorders and disturbances than PD-FOG patients. This included overall worse sleep quality, increased daytime sleepiness, and more disruptive sleep disturbances than those without FOG. Furthermore, PD+FOG patients had higher scores on several metrics measuring rapid eye movement behavior disorder (RBD), indicating a higher likelihood and increased severity of RBD in PD+FOG patients compared to PD-FOG patients. However, the study was limited by the heterogeneity in the scales used to assess sleep disturbances in PD patients. Nonetheless, the present study demonstrated the association between FOG and sleep disturbances in PD patients.
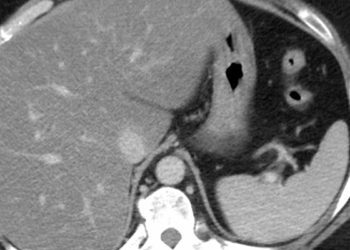
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.