Wellness Check: Sleep
Cognitive-behavioural therapy improves sleep in patients with mild cognitive impairment
1. In patients with mild cognitive impairment, empowerment-based cognitive behavioural therapy was shown to improve sleep and cognition after 6 months.
2. Patients receiving cognitive behavioural therapy had a greater reduction in insomnia and greater improvement in global cognition when compared to patients receiving standard care.
Evidence Rating Level: 1 (Excellent)
Mild cognitive impairment (MCI) is a transitional stage between normal aging and dementia. Sleep disturbance is an important risk factor for progression to further cognitive impairment. Non-pharmacological sleep-promoting interventions such as cognitive behavioural therapy (CBT) have been shown to improve sleep outcomes. However, the effectiveness of CBT in patients with MCI is unknown. This pilot study aimed to test the feasibility and effectiveness of CBT in improving sleep and cognition in persons with MCI.
The 60 study participants were recruited from elderly community centres in Hong Kong and all had MCI and chronic sleep problems meeting DSM-5 criteria. Participants with confirmed dementia, impaired communication, history of psychiatric or sleep disorders of organic causes, shift workers, or those known to use hypnotics or other medications that affect sleep in the past 2 weeks were excluded. 30 patients were randomized to the control group, where they received usual care. The 30 patients in the intervention group, received empowerment-based CBT delivered over 12 weeks. Group sessions outlined sleep education, with additional support on behavioural maintenance. The Pittsburg Sleep Quality Index (PSQI) was used subjectively to evaluate the quality of sleep while the Insomnia Severity Index (ISI-C) was used to determine perceived severity and distress from insomnia. A Fitbit wristband was given to participants to objectively measure sleep patterns including total time in bed, total sleep time, and sleep efficiency. A battery of neuropsychological tests evaluated global cognition. The primary outcome measures were the PSQI, ISI-C, and various tests for neurocognition.
After 6 months, the intervention group showed greater improvement in sleep quality and reduced insomnia severity as well as improvement in global cognition, processing speed, and attention when compared to the control group. Participants also reported high satisfaction with the design, content, and organization of the intervention, further demonstrating the feasibility of CBT. The study is limited by its convenience sample and predominant female population. Nonetheless, as a pilot study, it demonstrates that CBT can be effectively used to improve sleep in patients with MCI.
Model predicts workplace vigilance from single sleep using under-mattress sensor
1. A machine learning model was developed for estimating vigilance impairment for high-risk shift work occupations using only data from a single prior sleep period.
2. The model was found to be comparable to current fatigue prediction models that relied upon self-reported data and multi-night measurements.
Evidence Rating Level: 1 (Excellent)
The ability to predict vigilance impairment in shift workers is critical to reducing workplace errors and accidents. Current methods for evaluating vigilance involve infeasible self-reported data and laborious multi-night measurements. This study aimed to evaluate a new model for predicting shift work vigilance based on sleep data collected only one day prior using an under-mattress sleep sensor.
Twenty-four participants were recruited for the study using local advertisements. Individuals were included if they were between 18-65 years old, had no symptoms of a sleep disorder, had a typical bedtime of 22:00-00:30, a typical wake time of 07:00-09:00, had a sleep duration between 6 and 9 hours, consumed ≤3 caffeinated beverages per day, consumed ≤10 standard drinks per week, were non-smokers, had no current use of medications or drugs that affected sleep, had no shift work or international travel in the previous 6 months, and had no history of psychiatric, neurologic, cardiac, or respiratory disorders. Study participants came to the laboratory for two 8-day visits, 1 month apart. Each visit began with a flip to a night-shift schedule, involving simulated tasks from 12 am to 8 am. A psychomotor vigilance task (PVT) was administered 6 times throughout the night to evaluate reaction times, reaction speed, and number of lapses in attention. The Withings sleep analyser (WSA) was used underneath the mattress to estimate total sleep time, sleep efficiency, and wake after onset. This data was then utilized in machine learning models to predict PVT performance based on preceding sleep data. The primary outcome measure was reaction time and error on a psychomotor vigilance task.
The final model demonstrated moderate accuracy for predicting PVT performance and was found to be comparable with current models that typically require at least 5 days of consecutive data.
Although the sample size was relatively small, the model was still able to predict fatigue from a single preceding sleep recording, highlighting its efficiency and feasibility. The ability to easily and accurately estimate the vigilance of shift workers will be a valuable tool to manage work schedules to reduce workplace errors.
Habitual short sleepers with comorbidities at increased risk of long COVID
1. In people with pre-existing medical conditions, there is a higher risk of long COVID in short sleepers compared with average-length sleepers.
2. Increasing habitual sleep may be a potential modifiable risk factor for long COVID in people with pre-existing conditions.
Evidence Rating Level: 1 (Excellent)
The risk of long COVID-19—defined as persisting symptoms and long-term sequelae after a COVID-19 infection—has been linked to pre-existing conditions such as chronic obstructive pulmonary disease, anxiety, depression, heart disease, hypertension, and diabetes. Habitual short sleep duration has been known to impair immune function and increase all-cause mortality. However, whether the risk of developing long COVID varies by sleep duration remains to be studied.
This study analyzed data from a large, multinational, cross-sectional survey of 13,461 individuals with confirmed COVID-19. 1,542 individuals reported long COVID which was defined as a history of confirmed or probable SARS-CoV-2 infection with at least 1 symptom lasting for over 3 months. Of those who had long COVID, 945 reported pre-existing medical conditions. Nighttime sleep duration was classified into 3 categories; average if slept 6 to 9 hours per night, short-duration if slept less than 6 hours on average per night, and long-duration if slept more than 9 hours on average per night. Multivariate logistic regression analyses were conducted to examine the association between sleep duration and long COVID. The primary outcome measured was a risk of developing long COVID.
Compared to participants who reported average sleep duration, the risk of long COVID was 3-fold higher for those that reported short sleep duration. There were also significantly more individuals with pre-existing cardiac conditions in the short sleeper category when compared with average and long sleepers. A limitation of the study is recall bias due to self-reported sleep data from the participants. Nonetheless, this study suggests that increasing nighttime sleep to average duration may be a potential modifiable risk factor for long COVID in people with comorbidities.
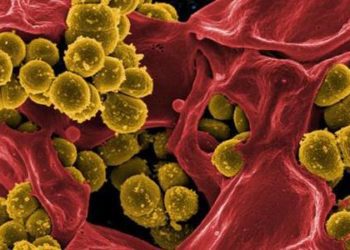
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.