The ZEUS study: everolimus maintains durable renal transplant function
1. Conversion at 4.5 months following kidney transplant from cyclosporine (a calcineurin inhibitor) to everolimus (a mTOR pathway inhibitor) maintains improved renal function at 5-year follow-up
2. Although post-conversion everolimus therapy was associated with an increased the rate of acute rejection, it was reversible and did not affect long term outcomes
Evidence Rating Level: 1 (Excellent)
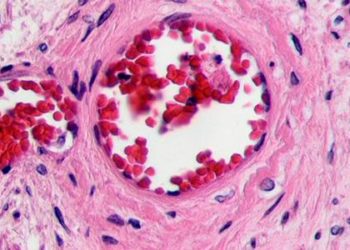
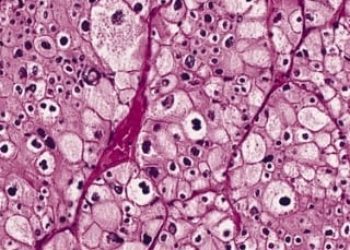
Study Rundown: Due to the significant nephrotoxic effects of Cyclosporine (CsA), a calcineurin inhibitor (CNI), the benefits of post-transplant immunosuppression on graft survival must be weighed against the risk of decreased graft function. Everolimus (an mTOR inhibitor) is less nephrotoxic and early conversion within the first 6 months post-transplant is linked to improved estimated glomerular filtration rate (eGFR) compared to CsA. Previous studies only showed short term 1-year follow-up of CNI sparing therapy while in the ZEUS study patients were followed for 5 years.
Strengths of the study included randomization to either CsA or everolimus, long term follow-up and post-hoc analysis of patients that remained in their study arm of immunosuppression during the study period. Limitations included the effects of acute rejection and adverse effects on graft survival when patients switched immunosuppressive regimen. Additional limitations included the low rate of monitoring for drug specific antibodies so the rate of chronic rejection could not be monitored.
Click to read the study in The American Journal of Transplantation
In-Depth [randomized controlled trial]: This study randomized 300 allograft kidney transplant recipients, 18-65 years of age, to either continue CsA or switch to everolimus at 4.5 months post-transplant. Estimated GFR was measured at baseline and at various time points for 5 years. Overall 5-year follow-up eGFR of everolimus was 5.3mL/min/1.73m^2 higher (95%CI 2.4, 8.3; p<0.001) than that of CsA. However, a number of patients switched immunosuppression due to acute rejection or adverse events. Therefore, in post-hoc analysis patients who remained in their study arm included 77/123 (62.6%) of everolimus and 84/109 (77.1%) of CsA patients. With adjustment for compliance, eGFR was higher for everolimus at 8.2mL/min/1.73m^2 (95% CI 4.3, 12.1; p<0.001). There was 21% loss to follow-up in the everolimus group and 25% loss to follow-up in the CsA group at the 5-year visit (reasons included withdrawing consent and death). Serious adverse events (pneumonia, UTI, nasopharyngitis and gastroenteritis) occurred in 17.4% vs. 11.7% of patients in the everolimus and CsA group respectively. Overall mortality of patients was low in both arms (<3%). Notably, the rate of acute rejection was far higher for everolimus (15.6%- majority Banff grade I) vs. CsA (7.5% p=0.032)
More from this author: Thromboelastography velocity better for predicting hyperfibrinolysis in trauma; Previous stroke may increase risk of complications after major surgery
Image: PD
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.