Surgical versus conventional therapy for weight loss treatment of obstructive sleep apnea [JAMA]
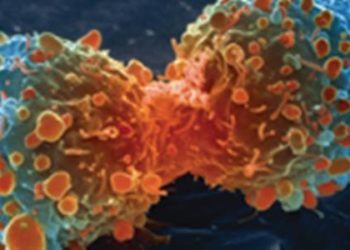
Image: CC/P. Prodoehl
Key Findings:
1. The study confirmed an association of weight loss with improved obstructive sleep apnea (OSA) but with variable individual effects
2. Use of surgical therapy compared to conventional therapy for weight loss did not demonstrate greater improvement of OSA in obese patients
Primer: OSA is strongly associated with obesity and related conditions, such as type 2 diabetes and hypertension. Moreover, patients with OSA have an increased risk of other morbidities, including stroke, cognitive dysfunction and reduced quality of life. One method of treating OSA is to use continuous positive airway pressure (CPAP), which aims to reduce upper airway resistance and prevent obstruction. Observational studies have shown that major weight loss may reduce OSA symptoms in up to 60-80% of patients. Medically supervised weight loss involves implementing a low-calorie diet, increasing physical activity, and having regular consultations with specialists, including a physician. Another approach to weight loss involves surgical intervention, and laparoscopic adjustable gastric banding (LAGB) has been shown to be a safe and effective surgical measure to lose weight. No randomized controlled trials have previously been conducted comparing medically supervised weight loss with bariatric surgery to treat OSA.
For further reading regarding the link between bariatric surgery and OSA, please see the following studies:
This [randomized controlled] study: Published recently in JAMA, a randomized controlled trial was conducted comparing medical weight loss to LAGB in improving OSA. The primary outcome was change in the apnea-hypopnea index (AHI) from baseline to 2 years as measured by diagnostic polysomnography. Secondary outcome measures included changes in weight and CPAP adherence. Both groups showed a significant decrease in AHI between baseline and 2 years. There was not a significantly greater improvement in AHI in the surgical group despite significantly greater weight loss compared with the conventional group. Post hoc analysis showed a significant positive relationship between change in weight and change in AHI.
In sum: While surgical intervention did result in greater weight loss compared to medical therapy, there was no significant difference in terms of improvement in OSA. The pattern of AHI improvement observed in this study indicates that benefit is associated with mild to moderate weight loss and limited additional benefit can be achieved through further weight loss.
Limitations of the study include the use of LAGB surgery as opposed to gastric bypass and biliopancreatic diversion, which have shown faster and greater mean weight loss. Furthermore, the study may have been underpowered due to the significant and unexpected variance in effect of weight loss on AHI. Additionally, patients investigated had moderate to severe OSA, and results may be different in individuals with less severe OSA.
Given these findings, there is insufficient evidence to support using surgical intervention rather than conventional medical weight loss therapy to improve OSA.
By AdC amnd AC
© 2012 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. DISCALIMER: Posts are not medical advice and are not intended as such. Please see a healthcare professional if you seek medical advice.